Colorectal cancer develops when an abnormal mass of cells develops in the colon or rectum. It is also known as colon cancer.
Colorectal cancer is the most common cancer among Malaysian men, inflicting about 15 in 100,000 men, and the second most common cancer among Malaysian women, inflicting about 11 in 100,000 women. It is also Malaysia's third leading cause of cancer deaths.
What causes colorectal (colon) cancer?
In most cases, colorectal cancer develops due to changes in the deoxyribonucleic acid (DNA) make-up of small growths (polyps) in the large intestine. These DNA mutations, combined with the failure of genes to discard mutated cells, will result in uncontrolled division and proliferation, and lead to tumour formation.
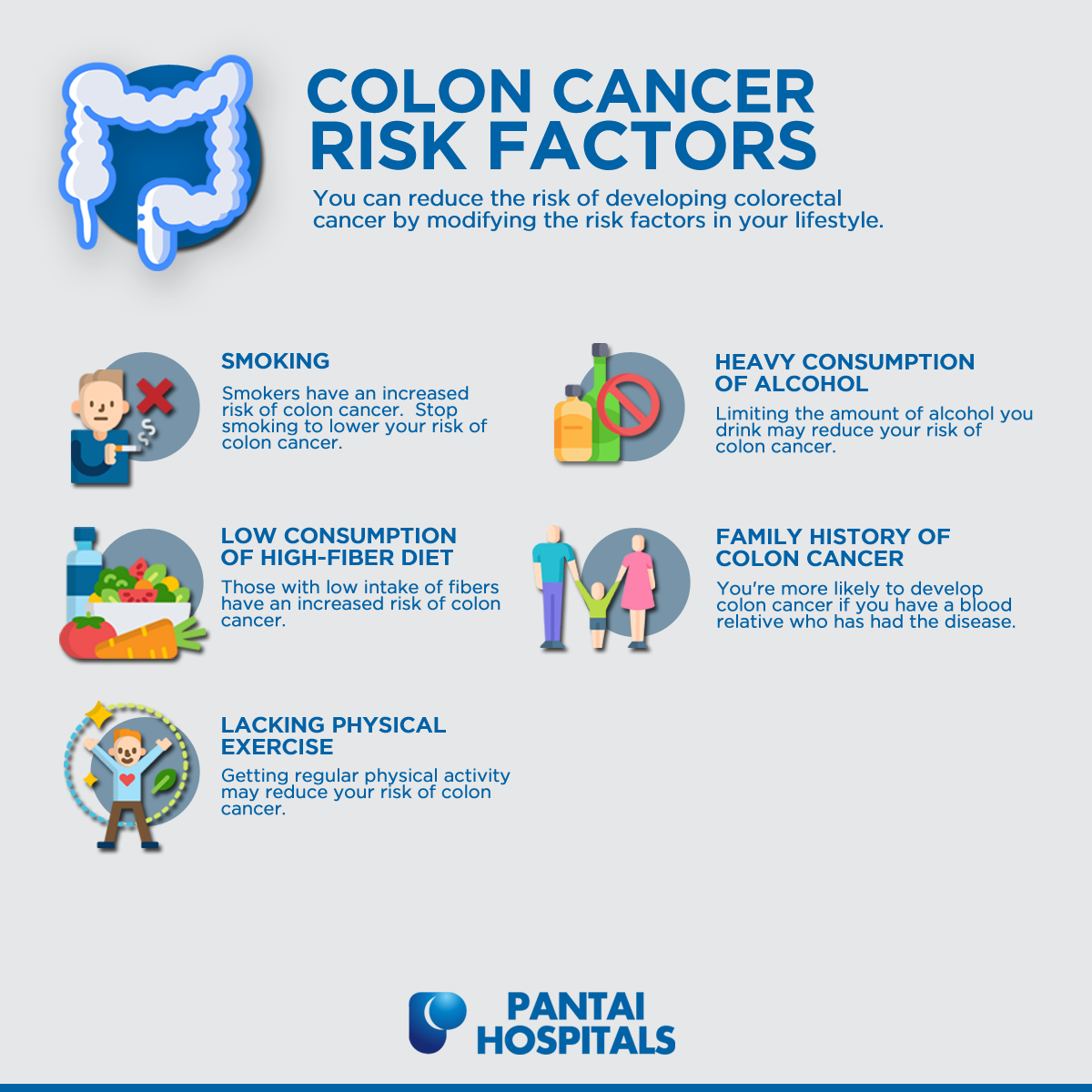
What are the risk factors of developing colorectal (colon) cancer?
The development of colorectal cancer is influenced by a complex interplay between a person’s genetic and environmental risk factors. Some common risk factors are:
The risk of developing this cancer is markedly increased after 50 years old. However, apart from the inheritance form of this condition, the onset of colorectal cancer below the age of fifty has become more common over the decade.
Having these underlying inflammatory bowel diseases (IBDs) increases the chance of developing this cancer. Chronic inflammation found in IBDs often produces an abnormal cell growth known as dysplasia.
Although dysplastic cells are not yet malignant, they have more chances of developing into a tumour. This risk increases a person’s overall carrier-span of the disease, as well as the level of severity of their inflammation.
Risk of colorectal cancer is increased if one has a blood relative with the disease. Those with two or more cancer-stricken first-degree relatives (parents or siblings) have a greater risk (two to threefold) of the disease, a group which accounts for about 20% of all cases.
A positive family history of colorectal cancer, especially in relatives under the age of 50 at point of diagnosis, confer an increased risk by way of inherited mutations and/or the environment.
About 5 in 100 people with colorectal cancer have a genetic condition that predisposes them to acquiring the disease, either in the form of familial adenomatous polyposis (FAP) or hereditary nonpolyposis colorectal cancer (HNPCC, or Lynch syndrome). These two are known to cause cancer at much younger ages. For those with these syndromes, cancer almost always occurs and makes up 1% of all cases.
- Male gender: Both global and local data show higher incidence in males compared to females
- Having a diet high in fats, red meat, and processed food, and low in fruits and vegetables (fibres): Low consumption of fibre increases risk of colon cancer
- Smoking: Quitting smoking can lower one's risk of colon cancer
- Heavy alcohol consumption: More than one drink a day increases risk of colon cancer
- Lack of exercise and obesity: Approximately 10% of cases are linked to insufficient activity
What are the signs and symptoms of colorectal (colon) cancer?
Early-stage colorectal cancer may not show obvious symptoms and is identified through active screening for colorectal cancer.
Some signs and symptoms of colorectal cancer are:
- Blood in stools
- Change in bowel pattern (diarrhoea or constipation)
- Change in stool consistency
- Unintentional weight loss
- Abdominal pain
- Vomiting
- Feeling that the bowel does not empty thoroughly after a bowel movement
- Fatigue
- Frequently having gas pains or cramps
- Feeling full or bloated
How do doctors diagnose colorectal (colon) cancer?
Different diagnostic tests are chosen by the doctors based on the type of cancer suspected, the age and general health of the person, signs and symptoms, results from earlier medical reports, and family medical history.
Common diagnostic tools include:
- Faecal Occult Blood Test (FOBT)
- Blood tests: Complete blood count, tumour markers and liver enzymes
- Colonoscopy
- Biopsy
- Imaging tests: Computed tomography (CT) scan, magnetic resonance imaging (MRI) scan, positron emission tomography (PET) scan
Learn more about the different types of screening and diagnostic procedures performed to diagnose colorectal (colon) cancer.
How is colorectal (colon) cancer treated?
In most cases, colon cancer originates as lumps of cells (known as polyps) within the colon which start turning malignant with time. Doctors can detect the polyps before they turn cancerous.
When cancer has gained substantial size over the years, it is not only able to invade the space of surrounding organs and blood vessels, but penetrate them, allowing the disease to spread.
Oncologists use a staging system to determine the extent of the spread of cancer and to formulate a suitable treatment methodology.
Treatment for colorectal cancer involves a multidisciplinary team approach such as colorectal surgeon, oncologist, radiation oncologist, and gastroenterologist.
Treatment options depend on the type, spread, and size of tumour. Following are the main treatment options adopted:
Most colorectal cancers will have to be removed with surgery.
- For early-stage colorectal cancer: Laparoscopic approach or polypectomy (removing polyps during a colonoscopy)
- For advanced stage colorectal cancer: Open surgery to remove the cancer and surrounding colon tissues and lymph nodes (glands)
Following are some commonly deployed treatment lines based on the stage of cancer:
- Stage 0: Surgery to remove the tumour growth.
- Stage 1: Surgery to remove the cancerous growth.
- Stage 2: Surgery is done to remove the cancerous growth followed by chemotherapy. This is required only in cases where cancer is suspected to be a high grade or if the patient has other health conditions.
- Stage 3: Surgical removal of tumour and affected lymph nodes followed by chemotherapy. For some patients, radiation therapy may also be suggested.
- Stage 4: Treatments could be a combination of surgery, chemotherapy, and sometimes radiation therapy. Doctors may also recommend immunotherapy and targeted therapy for some patients.
It is important to note that the treatment option is not singularly dependent on stage but may take into consideration other factors such as overall health of the patient, age, other co-existing medical conditions, etc.
In advanced stages where the great extent of cancer has been established at diagnosis, treatment is often directed at palliation (to relieve symptoms caused by the tumour and keep the person comfortable for as long as possible).
Palliative care includes:
- Maintenance of adequate nutrient intake through meal planning and care.
- Adequate pain management, mostly through pain medication.
- Maintenance of physical condition through some form of exercise, which may vary based on the patient’s age.
- Prevention of avoidable hospital admission (e.g., chest physiotherapy to prevent pneumonia).
- Psychosocial support from health professionals including mental health counselling, group-based support systems or spiritual support.
Learn more about the different types of treatment technologies to treat colorectal (colon) cancer.
What can I do to reduce the risk of developing colorectal (colon) cancer?
The following healthy habits can help prevent colorectal cancer:
- Eat a healthy balanced diet:
- Eat plenty of fibre-rich foods, fruits, vegetables, and whole grains.
- Reduce intake of red meat, processed foods and excessive charred or barbecued meat.
- Exercising regularly.
- Stop smoking and reduce alcohol intake.
- Maintain a healthy body weight.
- Consider getting screened to catch colorectal cancer early.
Frequently asked questions (FAQs)
Cyst is an air, fluid or semi-solid substance filled cavity which can develop in any part of the body including bones, organs, or soft tissues.
Polyp is an abnormal growth of tissue, protruding from the mucous membrane. Polyps are abnormal tissue growths which are most commonly found in the colon, but can also be found in the stomach, uterus, throat, and nose.
Don’t worry, blood alone isn’t a reason to panic. It could point to a number of things such as haemorrhoids, anal fissures, or other diseases. It is only when coupled with other colorectal cancer symptoms – irregular bowel movements, fatigue, sudden weight loss, feeling like your bowels have not emptied properly – that you should make a medical appointment as soon as you can.
The best method to check for polyps and colorectal cancer is colonoscopy. You will be sedated, and the doctor would view the entire colon using a long, flexible scope. If polyps are found, they can be removed during the procedure and tested for cancer.
Faecal occult blood test (FOBT) is a lab test that checks for the presence of blood in the stool. The stool is collected at home in sample tubes, which are then sent to a lab.
If you notice any changes in your bowel habits or if you notice any symptoms of colorectal cancer, do seek medical attention.
Prior to a colonoscopy, your doctor may advice you to clear your colon as the imagery of your colon and rectum may be blocked by any existing residue while you are being examined.
You may need to eat a specific diet prior to your examination day or consume a prescribed bowel preparation to assist in the clearing of your colon. Some patients use an enema kit to facilitate colon cleansing.
One of the preparations for colonoscopy involves wearing a gown and receiving sedation via an intravenous injection. This is designed to reduce any discomfort you may experience.
During the examination, the doctor will place you lying on your side on the exam table. The doctor will then insert a colonoscope into your rectum, which allows air to be pumped into your colon to facilitate a clearer view of your colon lining. You may feel abdominal cramping or the urge to pass motion movement whenever the scope is moved, or air is introduced.
The colonoscope has a tiny video camera at its tip, which is used to display images of the insides of your colon on an external monitor. Your doctor may also insert other instruments to take tissue samples (biopsies) from areas of abnormal tissue or remove polyps.
Myths & facts
Make an appointment at Pantai Hospitals
Early detection of colorectal (colon) cancer makes it easier to treat the disease with effective and appropriate treatment. A dedicated multidisciplinary team of specialists and oncologists at Pantai Hospitals is available for consultation to provide the best care and assistance to patients through screening, diagnosis, and treatment.
Get in touch with us to book an appointment today if you have any concerns or questions about colon cancer treatment options.
Pantai Hospitals have been accredited by the Malaysian Society for Quality in Health (MSQH) for its commitment to patient safety and service quality.

 Request an Appointment
Request an Appointment.webp?sfvrsn=276ce14_1/vector-(3).webp) International Patient
International Patient
.webp)
.png?sfvrsn=5eb4dd6e_9)
 Find A Doctor
Find A Doctor


.webp?sfvrsn=20763f7d_19)
.webp?sfvrsn=f2a2c343_9)